The Evolution of Understanding Fibromyalgia:
Dr. Don L. Goldenberg, MD
Chief of Rheumatology
Newton-Wellesley Hospital
While there wasn't much new territory covered, it was an interesting refresher course for me and a good deal of helpful information for my friend who was recently diagnosed with fibromyalgia. Here are some
highlights of the Fibromyalgia Symposium hosted by the Arthritis Foundation New England Region and Dr. Don Goldenberg, Chief of Rheumatology at Newton-Wellesley Hospital:
Most interesting quote: "Do not expect to get cured, but expect to get better." Dr. Don Goldenberg
Objective "Proof" of FM: Yes, Virginia, Fibromyalgia
DOES exist! On functional MRI's, pain receptive areas of the brain light up more in FM patients showing higher intensity to pain stimulus than a person without FM. Imaging technology is the wave of the future for pain research.
New Genetic Discovery: The S/S genotype of
5-HTT, the serotonin transporter gene which regulates pain and mood, is more common in people with FM. This genotype also increases the susceptibility to depression after stressful events. Its presence in some FM patients suggest altered serotonin metabolism in at least a subgroup of people with fibromyalgia.
Historical Factoid: Alfred Nobel, scientist and founder of the Nobel Prize, had paralyzing fatigue with rheumatic pains - in other words, fibromyalgia! Nobel said, "I am more seriously ill than my doctors think" to which Dr. Goldenberg replied, "He knows what he's talking about."
All in the Family: If you have fibromyalgia, it is 8.5 times more likely that fibromyalgia runs in your family. My aunt and two female cousins on my paternal grandmother's side also have fibromyalgia.
"Pain Thermostat" set too high: Dr. Goldenberg stressed that fibromyalgia is not a specific disease but a condition like hypertension which should be viewed on a spectrum. In Fibromyalgia patients the "pain thermostat" or "pain volume" is set too high creating a heightened pain response. On the scale between "no pain" on one end, "mild pain" in the middle and "chronic/severe pain" on the other end, FM patients fall on the extreme end of the pain spectrum.
Most interesting website: Recommended by Dr. Goldenberg,
knowfibro.com was developed by Lilly, a pharmaceutical company, but provides helpful information about fibromyalgia rather than promoting their products.
Most Interesting Headline: In 2009 three drugs were finally approved by the FDA for treatment of fibromyalgia. The headline in the New York Times read:
Drug Approved - IS DISEASE REAL? Dr. Goldenberg's comment to the audience of fibromyalgia patients was, "You guys still have to put up with that."
New e-book: Dr. Goldenberg assured us that we didn't have to take notes because all of his slides are covered in his new 400 page e-book,
FIBROMYALGIA: THE FINAL CHAPTER
which is available on Amazon for $9.99. The Kindle App is free to download and can be used to view the book on Kindle, i-pad/i-phone or any Mac or PC. So, if you weren't able to attend the symposium, you can still pick Dr. Goldenberg's brain through his e-book.
New Research Project 2011-2012: Dr. Goldenberg has received a grant from Pfizer to find out if early intervention can prevent severe fibromyalgia symptoms in the long-term. Dr. Goldenberg encourages primary care physicians to diagnose fibromyalgia earlier which means less tests, less medications, less specialists and hopefully less long-term suffering.
Overview of Dr. Goldenberg's Presentation:
Chronic widespread pain affects 5-15% of the population. Fibromyalgia, a subset of that group, affects 3-5% of the population around the world. There is no structural basis for fibromyalgia as there is in arthritis or spinal injuries. Fibromyalgia is the most common cause of "hurting all over." FM is not arthritis which is articular pain, both inflammatory (rheumatoid) and non-inflammatory (osteoarthritis). Fibromyalgia is
non-articular pain which is soft tissue pain. FM is not considered classically as a "disease" but a
functional illness in which there is a dysfunction in the body.
The peak age of onset of FM is between the ages of 35-60 and affects more women than men. However, FM affects all ages and genders and the rate of FM is the same in adolescents as in adults.
Without lab tests to make a diagnosis, FM is
diagnosed through symptoms such as widespread pain for more than three months, fatigue, irritability and cognition impairments. The three areas of diagnosis are: 1) no other systematic disease such as lupus or arthritis 2) chronic widespread pain and 3) tender points or trigger points. While the standard diagnosis used to be pain in 11 out of 18 trigger points, that system was too subjective and not used properly by doctors. The
American College of Rheumatology Classification Criteria of Fibromyalgia now includes the
Widespread Pain Index and
Symptom Severity Scale which takes into account more than just the tender points such as fatigue, morning stiffness, numbness and tingling, headaches, irritable bowel, anxiety and depression.
Dr. Goldenberg said that Lyme Disease is a big problem "in this neck of the woods" (pun intended) and felt that
chronic Lyme is probably fibromyalgia or chronic fatigue.
The most common scenario for the onset of FM is that a patient was totally healthy then suddenly got fibromyalgia. It can also be present since childhood or be the result of a specific event. It is more common in women than men but that could be a bias on the part of practitioners who are not diagnosing FM in men. However, not only do women have lower tolerance to pain than men (this is true across species as well) but chronic widespread pain occurs 2X more in women than men.
Precipitating factors: There is a genetic component to FM. In fact, it is 8X more common in families. Triggers of FM include the flu or a virus, a motor vehicle accident, stress, childhood abuse or some combination of the above.
Pathophysiology: FM is disordered pain processing, which is due to imbalances in hormones, the autonomic nervous system and the endocrine system. "Stressors" that aggrevate FM include injury, osteoarthritis, infection, PMS, psychological stress, steroid withdrawal and hormonal alteration such as hypothyroid. Menopause does not seem to change the severity of the symptoms. FM is diffuse
hyperalgesia, heightened pain response and/or
allodynia, pain from normally painless stimuli such as noise. FM patients have
4 to 5X greater pain response than normal individuals. Neural hormones central in stress reaction (fight or flight) which release cortisol are abnormal in FM. However, there is no "treatment" for this with medicaitons.
The
set point for stress is higher with FM and can be affected by genetics, gender, another disease, environmental causes, and/or negative life experiences. The higher the set point/the higher the stress, the more pain is experienced. Hopefully that stress point can be reset and brought down.
Non-restorative sleep: FM patients experience
Alpha Wave intrusion in which there is no Delta Wave, or restorative, sleep. When the sleep of normal patients was interrupted with noise they began to experience the pain and fatigue present in FM.
STAY TUNED FOR PART II & III: MOOD DISTURBANCES AND MANAGEMENT OF FM
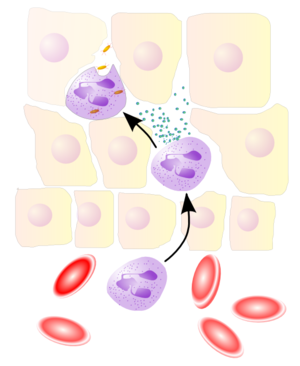 Image via Wikipedia
Image via Wikipedia